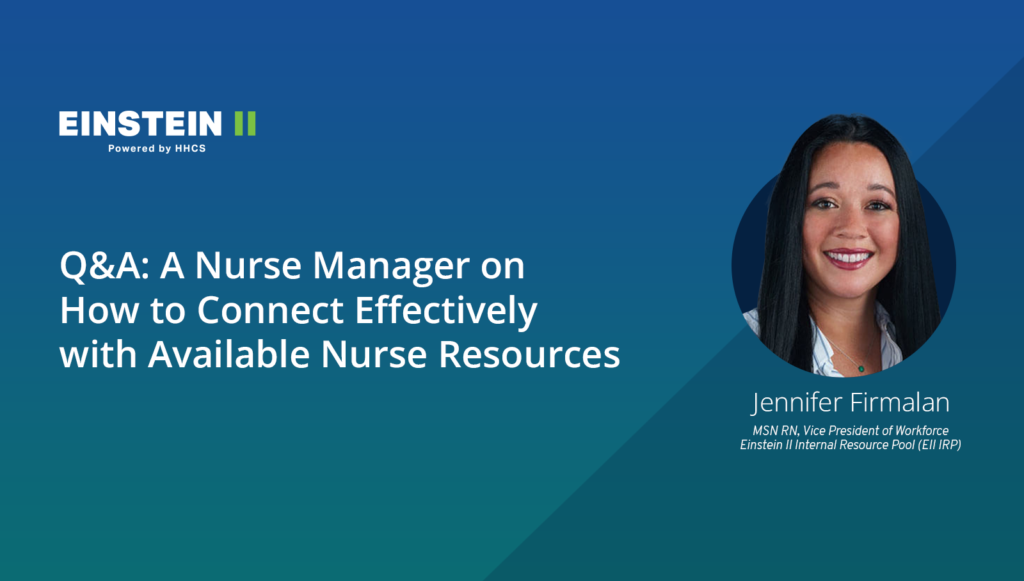
Jennifer Firmalan, MSN RN, is Vice President of Workforce for Einstein II Internal Resource Pool (EII IRP) at Hallmark Health Care Solutions (HHCS). Starting as a float pool nurse herself, Jennifer understands the staffing and deployment challenges hospitals face. Over the course of her career, she took on management roles overseeing float pool programs at multiple major health systems before joining HHCS. As a result, she offers a combination of expertise and experience uniquely well suited to finding, attracting, and managing contingent labor.
Today, Jennifer is answering questions about how hospitals and health systems can use float pools as a strategic tool to counter staff shortages and improve utilization of nurse labor.
Where does a float pool fit into a hospital’s response to the nurse labor shortage?
To start, it helps with retention. Nurses are leaving their positions in record numbers. Surveys from this year have found that nearly half (43%) of nurses are considering leaving their current roles, with some specialty areas even harder hit. As many as two-thirds of acute and critical care nurses are contemplating vacating their positions!
These nurses have childcare issues, are burned out, want to retire, don’t want the vaccine right now, want to work part-time instead of full-time, are taking on a second job, and on and on. These nurses often need to be able to pick their own shift because they’re working around their family’s schedule or other considerations. If they don’t have an option for flexible employment, they will just leave the organization. A float pool can give them a way to stay and get them back to the bedside … but only if the pool is built right.
How is a “built-right” float pool designed?
They’re designed for the nurses. When most hospitals and health systems design float pools, they’re typically trying to solve internal gaps and problems. That’s obviously important, but that doesn’t necessarily equate to “built-right.”. For example, a hospital wants to shore up understaffed shifts, so they require float pool nurses to work nights or every third weekend or a minimum total eight hours. These types of demands lower the likelihood that an organization can grow its program and increase the chances you’ll lose existing nurse resources because they find the flexibility they want elsewhere.
We have to change the traditional outlook on float pools and instead look at it from the nurse’s perspective. That means the question isn’t what you want from them, it’s what does the nurse want from you?
The same dynamic applies to attracting new experienced nurses into the float pool program.
Maybe there’s a nurse who’s employed elsewhere but wants to pick up extra shifts or would like to take a “try before they buy” approach to working for you. Reducing the barriers to entry and giving nurses what they want – the flexibility of a “gig” style employment model – solves a problem for them as much as for the hospital and maximizes engagement with the float pool program.
Does revamping a float pool program really make that much of a difference?
A strong float pool program will better connect supply and demand. One critical factor: you can build a great float pool but if it doesn’t have the right technology to quickly communicate open needs and track utilization, you’ll face an immediate barrier to success.
Speaking from personal experience, when I first worked in a float pool, we used legacy scheduling software to manage it. But it had so many restrictions about even getting into the system, I’d forget about the shifts scheduled far in advance, then I couldn’t find out what days I was supposed to work, and no one and nothing communicated that information to me.
Then our float pool program got on Einstein II Internal Resource Pool (EII IRP) technology. Without even having to call in, I could schedule a shift myself and receive automated notifications and reminders. It was so much easier to connect than the previous way. My colleagues and I also became more productive at that point, because any of us at any point in time could easily say, “I have 8 hours available, and pick up a shift.”
I’m not the only one with that kind of experience. One EII IRP user, a health system based in Tennessee, tripled the size of its float pool in the first three months. Another was able to significantly boost productivity. The combination of a larger float pool and better utilization then naturally leads to reduced agency spend (in one case saving one health system as much as $13.5 million net annually). The right technological underpinning makes all the difference. In the end, a well-built float pool is a superb mechanism for creating long-term staff sustainability. Knowing you have a bench of resources available eases turnover because you always know you have someone else to fall back on.